Abstract
Background: Prior work has shown that multivariable models can have reasonably high accuracy in predicting early deaths (deaths within 28 days of starting induction, defined as treatment-related mortality [TRM]) following intensive AML chemotherapy. These models can be used to derive a TRM score reflective of the probability of TRM with intensive AML therapy, and such scores can be used to make informed treatment decisions and as explicit eligibility criteria in AML protocols. The degree to which non-fatal toxicities can be predicted is unknown. It is also not known which patient characteristics are most strongly associated with occurrence of non-fatal toxicities following induction chemotherapy. Here, we examined these questions using data from the most recent SWOG Phase III with a 7+3 arm.
Patients and Methods: We analyzed 260 eligible patients randomized to the 7+3 arm SWOG trial S1203 who received the first cycle of protocol therapy. 7+3 was per contemporary standard when the trial was opened in 2012: 100mg/m2 cytarabine on days 1-7 and 90mg/m2daunorubicin on days 1-3. Toxicities were reported using CTCAE version 4.0. We used logistic regression models to model toxicity incidence and evaluated the predictive accuracy of the models with the area under the receiver operating characteristic curve (AUC). We note that AUC of 0.5 is what would be expected with random chance or using a coin flip to make a decision, while an AUC of 1 denoted perfect prediction. We evaluated the following baseline covariates (modeled quantitatively unless otherwise specified): age at study registration, gender, Zubrod performance status (0-1 versus 2-3), pre-study white blood cell counts (WBC), pre-study platelets, pre-study marrow blasts, secondary vs. de novo AML, cytogenetic risk, and NPM1+ and FLT3-ITD- versus other NPM1/FLT3-ITD status. For toxicities with lower incidence, the number of covariates included in multivariable models was proportionate to one covariate per 10-15 patients with a toxicity. Toxicities were reported using the contemporary CTCAE version 4.0. Only toxicities observed during the first cycle of induction are analyzed below.
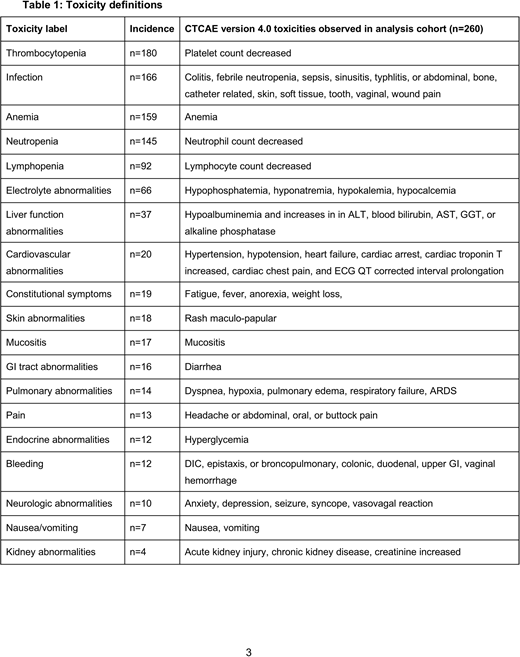
Results: We evaluated the incidence grade 3 or higher thrombocytopenia (n=180, 70%), infection (n=166, 64%), anemia (n=159, 61%), neutropenia (n=145, 56%), lymphopenia (n=92, 35%), electrolyte abnormalities (n=66, 25%), liver abnormalities (n=37, 14%), cardiovascular abnormalities (n=20, 8%), constitutional symptoms (n=19, 7%), skin abnormalities (n=18, 7%), mucositis (n=17, 7%), GI tract abnormalities (n=16, 6%), pulmonary abnormalities (n=14, 5%), pain (n=13, 5%), endocrine abnormalities (n=12, 5%), bleeding (n=12, 5%), neurologic abnormalities (n=10, 4%), nausea/vomiting (n=7, 3%), kidney abnormalities (n=4, 2%).
In univariate models no individual covariate was a strong predictor of toxicity. Only 3 pairs of toxicity/covariate had an AUC > 0.65 [indicating modest predictive ability]: older age predicting increased risk of endocrine abnormalities (OR=1.08 [per year], p=0.06, AUC=0.67), higher baseline WBC predicting increased risk for bleeding (OR=1.26 per 1,000, p=0.36, AUC=0.67), and higher baseline HGB predicting increased risk of neurologic toxicity (OR=1.33 per g/dL, p=0.10, AUC=0.69).
As incidence allowed, we evaluate multivariable models. Multivariable models had increased AUC compared to univariate models, but no multivariable model had an AUC larger than 0.70.
Conclusion: These findings indicate that with the baseline covariates evaluated, we have a poor ability to predict commonly occurring grade 3 and higher toxicities that occur during the first cycle of 7+3 induction therapy for AML. These findings support the claim that randomization is necessary to compare toxicities between standard and investigational regimens. Moreover, assuming that trial eligibility criteria are often stringent in an attempt to minimize the occurrence of treatment toxicities in study participants, the lack of strong association between individual baseline characteristics and toxicities could be used to argue for less-stringent study inclusion criteria.
Support: NIH/NCI grants CA180888 and CA180819
Walter:Aptevo Therapeutics, Inc: Consultancy, Other: Clinical Trial Support, Research Funding; Amphivena Therapeutics, Inc: Consultancy, Other: Clinical Trial Support, Research Funding; Covagen AG: Consultancy, Other: Clinical Trial Support, Research Funding; Seattle Genetics, Inc: Consultancy, Other: Clinical Trial Support, Research Funding; Pfizer, Inc: Consultancy; Amgen Inc: Other: Clinical Trial Support, Research Funding; Actinium Pharmaceuticals, Inc: Other: Clinical Trial support , Research Funding; Boehringer Ingelheim Pharma GmbH & Co. KG: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal